各種活動
小児のコロナウイルス感染症2019(COVID-19)に関する医学的知見の現状
日本小児科学会 予防接種・感染症対策委員会
2020年11月11日 第2報
要 旨
- COVID-19患者の中で小児が占める割合は少ないが、感染の拡大に伴ってその割合が増えてきた。
- 学校や保育所におけるクラスターは起こっているが、社会全体から見ると多くなく、小児COVID-19症例の多くは家族からの感染である。
- 小児は成人と比べて感染しにくい可能性が示唆された。
- 小児COVID-19症例のSARS-CoV-2排泄量は、成人と比べて同程度である。
- 小児COVID-19症例では、SARS-CoV-2は鼻咽頭よりも便中に長期間そして大量に排泄される。
- 小児COVID-19症例は成人例と比べ軽症であり、死亡例はほとんどない。
- ほとんどの小児COVID-19症例は経過観察または対症療法が選択されている。
- 小児では抗体が検出されるようになってもウイルスの排泄が続いていることがある。
- 他の病原体との混合感染も少なくない。
- COVID-19罹患妊婦は非罹患妊婦よりも集中管理を要する可能性が高くなる。
- SARS-CoV-2の垂直感染は稀で、児の予後は良好である。しかし、新生児の感染は重篤化する可能性も報告されている。
- 海外の数理モデリング研究や系統的レビューでは、学校や保育施設の閉鎖は流行阻止効果に乏しい可能性が指摘されている。
- 教育・保育・療育・医療福祉施設等の閉鎖や大人(養育者)のストレスが小児の心身に影響を及ぼしており、COVID-19流行による周りの環境変化に関連した健康被害が問題となっている。
疫 学
COVID-19 患者において小児の占める割合は少ないが、増加傾向にある
- 小児の感染者数は少なく、その割合は中国では19歳未満の患者は全体の2.4% [1]、米国では2020年4月2日の時点で18歳未満の患者は全体の1.7% [2]、日本国内では5月3日の時点で10歳未満が1.6%、10~19歳が2.3%だった [3]。しかし次第に小児の割合が増えて来ており、米国では10月10日の時点で18歳未満は全体の8.8% [4]と報告され、日本国内でも10月7日の時点で10歳未満の患者総数は2,112人 (2.4%)、10~19 歳では4,399人 (5.1%) と報告されている [5]。
小児例の多くは家族内感染である
- 家族の中で小児が先行感染者になることは少なく、中国における家族内感染の調査では8%に過ぎなかった [6]。5月28日までに発表された1,099本の論文のスコーピング・レビューにおいて、小児のCOVID-19の75~100%は家族内感染だった [7]。本学会による国内小児症例のレジストリーのデータ(2020年10月13日時点)でも、77%の小児症例は家族(特に親)から感染していた [8]。
学校や保育所におけるクラスターが報告されるようになったが、社会全体から見ると多くない
- 前述のスコーピング・レビューにおいて、小児は学校内の伝播にほとんど関わっていないことが示された [7]。オーストラリアからの報告では、15の学校で18人の患者 (9人は生徒、9人は学校職員) が 863人 (生徒735人、職員128人) と濃厚接触があったにもかかわらず、感染が確認されたのは生徒2人だけであった [9]。アイルランドやシンガポールでも学校閉鎖前に行われた調査で、学校内での二次感染例は非常に少なかったと報告している [10, 11]。ヨーロッパでは、9歳の患者が3つの学校やスキー学校で有症状のまま112名に接触したにもかかわらず、誰にも感染させていない事例もあった [12]。
- 米国ロードアイランド州ではsocial distancingや職員のuniversal masking等を厳格に実施した保育所666施設(全体の75%)で保育再開した後、COVID-19の発生が起こったのは29施設、そこで二次感染まで起こったのは4施設(全施設の0.6%)のみであった [13]。さらに全米5万7千人の保育施設スタッフへの調査で、パンデミックの初期(5月末〜6月初め)の保育施設の開設状況、感染予防策、そしてSARS-CoV-2感染の有無を調べ、感染者427人と非感染者、そして対照者との比較を行った。その結果、保育に従事していたことは感染のリスクに関与していなかった [14]。
- 日本におけるクラスターの発生件数は、内閣官房新型コロナウイルス感染症対策推進室によると7月から10月21日までの時点で1,352箇所に上る [15] 。一方、学校現場でのクラスターは9月3日時点までの累積で、小学校で3件、中学校で5件、高等学校で10件、特別支援学校で0件と報告されており、社会全体に起こっているクラスター件数から見ると少ない [16]。また感染経路を見てみると、小学生では家族内感染が75%に対し学校内感染が2%、中学生では家族内感染が68%に対し学校内感染が7%、高校生では家族内感染が32%に対し学校内感染が33%と報告されており、小中学校においては学校の中での感染というよりも、家庭から学校に持ち込まれたケースが圧倒的に多い [16]。
小児は成人より感染しにくい可能性がある
- 小児が成人と比べて感染しにくいのかどうか様々な報告が出ていたが、系統的レビュー/メタ分析の結果、オッズ比0.56(95%信頼区間 0.37-0.85)で成人より感染しにくい可能性が示唆された [17]。
- 世帯の223人の成人発端者からの家族内伝播を調べた研究では、7世帯 (5.2%)の13人(6.1%)に感染が及んだが、年齢層別にみると5歳未満では1.3%、5~9歳では8.1%、10~16歳では9.8%であり、低年齢では感染率が低かった [18]。
- SARS-CoV-2の受容体となるACE2の発現レベルが低く [19]、またSARS-CoV-2感染児は非感染児と比べてACE2発現度が高い傾向にあることも示されており [20]、ACE2の発現レベルがSARS-CoV-2への感染しやすさに影響していることが示唆されている。
小児からの感染力が成人より強いかは、まだ不明である
- SARS-CoV-2の排泄量を比べた研究がいくつかあるが、相反する結果を報告している。小児のウイルス排泄量が少ないと報告するもの [21]、0~22歳の間ではウイルス量に大差なかったと報告するもの [20] がある反面、5歳未満児では5~17歳の年長児や18~65歳の年齢層と比べてウイルス量が10~100倍多いという報告もある(ただしこの研究では無症候性感染児を解析の対象から除いている) [22]。
- [10-13] や、韓国における家族内伝播の研究で18歳未満小児107人からの家族内二次感染が1例しか起こらなかった報告は、小児が感染源となりにくいことを示唆している [23]。2020年5月11日までの報告をまとめた系統的レビューでは、小児は流行の中心とはなっていないことが示されている [21]。しかし、小児が成人よりも感染させにくいかどうかについては、結論が出せるだけのデータは揃っていない [17]。
臨 床
小児 COVID-19 症例は無症状〜軽症が多く、死亡例は少ない
- 小児COVID-19に関する中国・シンガポールからの18論文の系統的レビューで1,065症例(うち0~9歳は444例)を検討した結果、臨床症状は発熱、乾性咳嗽、全身倦怠感、嘔吐、下痢などで、発症後1~2週間以内に改善することが多かった [24]。0~9歳で集中治療を要した症例は1歳児の1例のみで、死亡例はなかった。米国の報告でも18歳未満では成人と比べて入院例が少なく(5.7~20%)、ICU入室の割合も低かった(0.58~2.0%) [2]。
- 日本国内では、10月7日の時点で10歳未満の患者2,112人、10~19歳の患者4,399人で死亡例はない [5]。5月28日までに感染症発生動向調査に届出があった0~14歳患者290人と15~19歳患者208人のうち、重篤な肺炎を合併したのは15〜19歳患者の2人 (1.0%) だけであった [25]。
- 米国では、小児の中でも1歳未満児と基礎疾患を有する児は、入院する頻度が高いと報告された [2]。中国では、年齢群を3歳未満、3~6歳、6~14歳に分けて比べると3歳未満では比較的症状が重く、3~6歳が最も軽かった [26]。イタリアでは、18歳未満の小児患者3,836人のうち4人(0~1歳で2人、2~6歳で2人)が死亡しているが、いずれも心血管系異常や悪性腫瘍などの重篤な基礎疾患を有し、COVID-19は原死因とは考えられていない [27]。
小児 COVID-19 の臨床的特徴
- COVID-19小児患者2,597例(24論文)のレビューでは、全体に症状は軽く、重症例は4.4%、重篤例は0.9%だった。初発症状は成人と同様であるものの 低頻度で、発熱は43.1% (成人では82~98.6%)、咳は43.4% (同59.4~82%)、多呼吸・息切れは12.6% (同31%) であり、呼吸困難や呼吸窮迫症候群の合併は稀である。一方で、消化器症状は成人と比べて多く、下痢は6.6% (同2~3.8%) だった。検査所見では、成人でよく見られるリンパ球減少は9.8%にしか認められず、その一方でクレアチンキナーゼMBアイソザイム(CK-MB)の上昇が27%と高率に認められた [28]。成人COVID-19患者で特徴的とされる嗅覚・味覚障害は、小児では自分から訴えることが難しいこともあって実態は不明だが、フランスの報告では18歳未満の症例の5.2%に認められている [29]。また香港からの報告では嗅覚・味覚障害のみを症状とする10代患者3人の報告もある [30]。
- 他の呼吸器病原体(マイコプラズマ、インフルエンザ、RSウイルスなど)との混合感染が稀ならず認められており、他の病原体が検出されてもCOVID-19を否定することにならない [26, 31]。
COVID-19関連小児多系統炎症性症候群
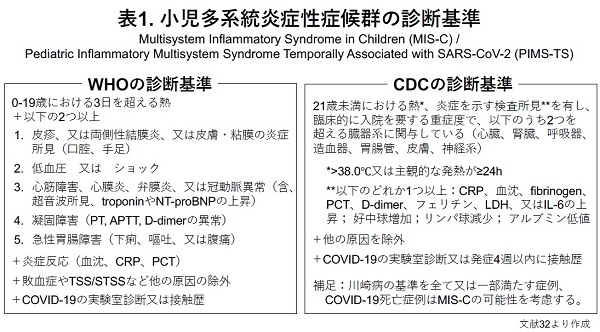
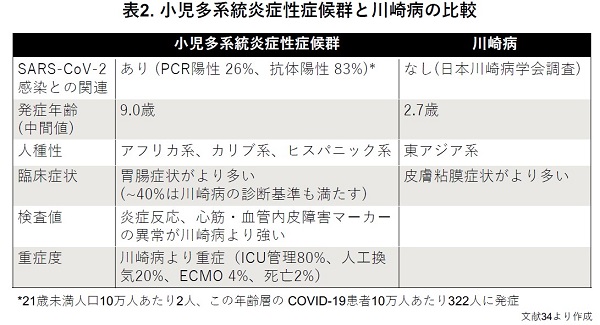
- 欧米等からは小児 COVID-19 に関連して、毒素性ショック症候群または (不全型) 川崎病を疑わせるような多臓器系にわたる強い炎症を起こす病態が発症しており、multisystem inflammatory syndrome in children (MIS-C)またはpediatric inflammatory multisystem syndrome (PIMS)という名称が提唱され、WHOとCDCがそれぞれ診断基準を出している(表1)[32]。
- SARS-CoV-2 PCR陽性率は高くない (26%)が、SARS-CoV-2抗体は83%で陽性である [33]。
- 川崎病より年長で発症し、人種的な背景も大きく異なり、臨床的にも胃腸症状が多く、皮膚粘膜症状は少ないなどの違いがあり、炎症反応や心筋・血管内皮傷害マーカーの上昇がより顕著で、重症度が高い(表2)[32-35]。
- 治療には人工呼吸器や血管作動薬などによる全身管理に加え、副腎皮質ステロイド、免疫グロブリン製剤、生物学的製剤(IL-6阻害薬やIL-1阻害薬 など)が用いられている [32-35]。
- 現時点では、国内で COVID-19 流行に伴って川崎病の発症数の増加はなく、MIS-C/PIMSが疑われる症例は報告されていない [36]。ただし、COVID-19のために入院した後で川崎病を発症した1歳児が経験されている [37]。
検査(含、ウイルスの動態と免疫応答)
SARS-CoV-2 は鼻咽頭よりも便中に長期間そして大量に排泄される
- COVID-19患者の気道および消化管からのSARS-CoV-2排出期間を検討した系統的レビューで、RT-PCRにより鼻咽頭あるいは咽頭スワブ検体からは発症から平均11.1日間、最大で24日まで検出された。一方、直腸スワブ検体では陽性率86%で、平均23.6日間、最大4週間検出された。89%の症例では、呼吸器検体より便検体から長期に渡りウイルスが検出された [38]。
抗体が陽性になった時点でもSARS-CoV-2が検出される。また再感染が阻止できる抗体価に達するのは約半数に過ぎない
- 22歳以下の小児及び若年成人215人に対してSARS-CoV-2 RT-PCRと抗体検査の両方を実施した研究で、33人(15%)ではウイルスRNAと抗体の両方が検出された。PCRが陰性になるまでの期間中央値は25日、SARS-CoV-2に対する抗体が出来るまでの期間中央値は18日で、中和抗体価が再感染阻止可能なレベル (80AU/mL)に達したのは52%に過ぎず、それに要した期間中央値は36日だった。小児においては抗体が検出されるようになった時点でもウイルスを伝播させる恐れがある [39]。
治 療
ほとんどの小児 COVID-19 症例は経過観察または対症療法が選択されている
- 小児のCOVID-19はほとんどの場合、成人と比べて軽症であることから、経過観察または対症療法が選択されている。本学会による国内小児症例のレジストリーのデータでも、508登録症例のうち446例は無治療で、それ以外も5例で吸入ステロイド剤、3例で静注ステロイド剤が用いられた症例を除くと対症療法のみで、抗ウイルス薬が用いられた症例はなかった [8]。
- 世界中で様々な治療薬が用いられて来たが、多くの薬剤は有効性や安全性のデータが不十分で、成人領域でも現時点でエビデンスが示された治療薬は、抗ウイルス薬のレムデシビルと副腎皮質ステロイドのデキサメタゾンのみである。小児ではいずれの治療法も使用経験が少なく、有効性や安全性のエビデンスは十分とは言えない [40]。
新生児
COVID-19 罹患妊娠・分娩において母体は集中管理を要するリスクが高く、早産になることが増えるが、垂直感染は稀である
- COVID-19罹患妊婦と出生児について2020年4月19日までに発表された33の論文の系統的レビューでは、385人の妊婦のほとんどが軽症で、重症例は3.6%、重篤例は0.8%だった。252人が分娩 (帝王切開69.4%、経腟分娩30.6%)に至り、出生した256人の新生児のうちPCR陽性が4名 (いずれも帝王切開出生) であったが、全て軽症であった。PCR陽性の新生児は母親由来のウイルスによる偽陽性の可能性もあるが、垂直感染は除外できない [41]。
- 6月26日までに発表された77の論文についての系統的レビュー/メタ分析では、COVID-19罹患妊婦は非罹患妊婦と比べて集中管理が必要となる可能性が高いことが示された (ICU入室のオッズ比1.62 [95%信頼区間1.33-1.96]、人工呼吸管理のオッズ比1.88 [1.36-2.60])。重症化に関わる因子として、高齢、肥満、基礎疾患(妊娠以前からの高血圧や糖尿病)の存在が挙げられた。また、早産率もCOVID-19罹患妊婦では6% [95%信頼区間3-9%]と、非罹患妊婦より高かった (オッズ比3.01 [1.16-7.85]) [42]。
- SARS-CoV-2陽性母体から出生した児への垂直感染に関する385の文献のうち17文献をメタ分析した報告では、402人の母体から生まれた405人の児のうちの330人に対して早期にPCR検査が行われ、9人が陽性でそのうち1人は出生時から症状を有していたため、子宮内感染と考えられた。ランダム効果モデル分析では、垂直感染率1.6% [95%信頼区間0.34-7.31]と考えられた [43]。
現時点で経母乳感染の証拠はない
- 先述の系統的レビューでは母乳の検査も26例について行われたが、SARS-CoV-2 PCRは全て陰性であった [41]。その他の報告をまとめると、24人中4人の母体の母乳10検体からSARS-CoV-2 RNAが検出されているが、いずれの場合も環境や感染した児からの汚染の可能性は否定されておらず、RNAの存在は必ずしも感染性であることを示してはいない。18人のSARS-CoV-2感染妊婦からの母乳検体に対して、経時的にPCRと細胞培養によるウイルス分離を行った研究では、1検体のみPCR陽性となったが、ウイルスは分離されなかった [44]。
- 単一分娩施設において、周産期にSARS-CoV-2に感染した妊婦から生まれた101人の新生児を全員母子同室で直接母乳哺育を行ったが、発症した児はいなかった [45]。
- このように、これまで行われていた母子分離や直接母乳哺育の制限を見直すことも検討できるかもしれない [委員会からのコメント]。
新生児が重症化しやすいかどうかはまだわかっていない
- 27のCOVID-19児の報告では、軽症ではあったものの、母親と比べてウイルスの排泄量が非常に多く、しかも鼻咽頭や唾液や便だけではなく血漿や尿からも検出されており、新生児では SARS-CoV-2 感染が全身に拡がる可能性が示された [46]。NICUにおける多施設前方視的研究では、COVID-19新生児症例37例(いずれも市中感染と思われる)のうち、41%に酸素投与、16%に非侵襲的呼吸管理、そして3%に人工換気が行われ、ダウン症候群と先天性心疾患を合併していた 1例が死亡した [47]。
COVID-19 流行期の子どもの心身の健康
学校や保育施設の閉鎖は流行阻止効果に乏しい
- 学校や保育現場において小児が感染源となったクラスターの報告は、国内外を通じて少ない。学校や保育施設での子どもの感染が契機となって家庭を介し社会へと流行が拡大していくインフルエンザの場合とは異なり、これまでに観察されたCOVID-19の流行拡大様式では社会での流行が家庭に持ち込まれて子どもが感染し、そこから学校や保育施設に拡大していくことが多い [16]。
- 流行に対する学校閉鎖の有効性について、数理モデリングで検討した研究や系統的レビューでは、学校閉鎖を行う事は、その他のsocial distancing などの感染予防措置と比べて効果は少なく [48-51]、COVID-19死亡者の減少は2~3%に留まっている。一方、子どもを養育している医療従事者も就業困難となり、結果的に医療資源が失われCOVID-19死亡者をむしろ増加させる可能性もあると考えられる [49]。
- Imperial College Londonによる数理モデリングによると、子ども・若年者の隔離はその後の流行を遅らせる効果がある反面、最終的には高齢者の死亡数を増加させるとしている。さらに、重症化が稀な子ども・若年層に感染者をとどめておき、感染すると致命率が高い高齢者に対して厳格なsocial distancingを求めることが、死者数を減らすには有効と推測している [52]。
- physical distancing介入(学校閉鎖、職場閉鎖、公共交通機関の閉鎖、大規模集会と公共イベントの制限、ロックダウン)を行った149の国・地域の検討において、COVID-19発生率が13%減少 (IRR 0.87 [95%信頼区間0.85-0.89])すると報告されているが、これらの介入は同時に組み合わせて実施されているため、学校閉鎖の効果を抜き出して示すことはできない [53]。米国において、学校閉鎖に伴ってCOVID-19患者数が62%、死亡数が58%減ったとする報告があるが、これも学校閉鎖と同時に他にも様々な感染拡大介入措置が取られていたため、実際のところどの介入措置がどの程度有効だったのかは解析できず、学校閉鎖の効果は不明である [54]。
教育・保育・療育・医療福祉施設等の閉鎖が子どもの心身に影響を及ぼしている
- 学校閉鎖は、単に子どもの教育の機会を奪うだけではなく、屋外活動や社会的交流が減少することとも相まって、子どもを抑うつ傾向に陥らせている [55, 56]。
- 療育施設では密な環境でのケアが避けられないため、COVID-19が発生すると施設内に蔓延しやすい。一方、療育施設の閉鎖により受け入れが困難になった医療的ケア児への対応が世界的に求められている [57]。
- 就業や外出の制限のために親子とも自宅に引き籠るようになって、ストレスが高まることから家庭内暴力や子ども虐待のリスクが増すことが危惧されている。加えて、対応する福祉施設職員が通常通り就業できない状況が虐待増加に拍車をかけている [58, 59]。
- 「子ども貧困」問題がクローズアップされている中、養育者の失業や収入減のために状況はさらに悪化している上、福祉活動や「子ども食堂」などのボランティア活動も滞っている [60]。
- 乳幼児健診の受診が減少し、子どもの心身の健康上の問題を早期に発見し介入することが制限され、大きな健康被害やQOLの低下に繋がることも危惧されている [61]。
- 予防接種の機会を失う小児が増えている事も大きな問題となっている。世界的にも1億2千万人近い子ども達が麻疹ワクチンの接種を受けることができない状況が危惧されている。ワクチンで予防可能な疾患に罹患してしまうことによる被害は甚大となる [62]。実際わが国においても、COVID-19流行下での予防接種の差し控えが起こっており [63]、ワクチン未接種の乳児が重症百日咳を発症したことが報告されている [64]。
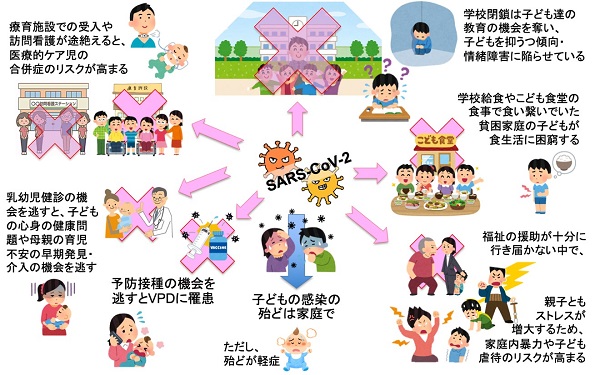
- 子どもでは、COVID-19が直接もたらす影響よりもCOVID-19関連健康被害の方が大きくなることが予想される(図)。
図.知見のまとめ:子どもの COVID-19 関連健康被害 (日本小児科学会予防接種・感染症対策委員会作成)
子どもは多くの場合、家庭で感染しているが、幸いほとんどの症例は軽症である。しかし、COVID-19 流行に伴う社会の変化の中で様々な被害を被っている。
引用文献
1. Jiatong S, Lanqin L, Wenjun L: COVID-19 epidemic: disease characteristics in children. J Med Virol. 2020 Mar 31. doi: 10.1002/jmv.25807.https://onlinelibrary.wiley.com/doi/abs/10.1002/jmv.25807
2. CDC COVID-19 Response Team: Coronavirus disease 2019 in children - United States, February 12–April 2, 2020. MMWR 2020; 69(14): 422–6.https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6914e4-H.pdf
3. 厚生労働省:新型コロナウイルス感染症の国内発生動向(令和2年5月3日18時時点). https://www.mhlw.go.jp/content/10906000/000627541.pdf (2020年5月5日アクセス)
4. CDC COVID-19 Data Tracker. https://covid.cdc.gov/covid-data-tracker/#demographics (2020年10月11日アクセス)
5. 厚生労働省:新型コロナウイルス感染症の国内発生動向(令和2年10月7日18時時点). https://www.mhlw.go.jp/content/10906000/000680684.pdf (2020年10月11日アクセス)
6. Posfay-Barbe KM, Wagner N, Gauthey M, et al: COVID-19 in children and the dynamics of infection in families. Pediatrics. 2020; 146: e20201576. DOI:https://doi.org/10.1542/peds.2020-1576
7. Rajmil L: Role of children in the transmission of the COVID-19 pandemic: a rapid scoping review. BMJ Paediatr Open. 2020; 4: e000722. DOI:10.1136/bmjpo-2020-000722.
8. 日本小児科学会:COVID-19日本国内における小児症例.https://www.coreregistry.jp/CoreRegistry_COVID19_CRF_Dashboard/Home/DashBoardviewer (2020年10月13日アクセス)
9. Macartney K, Quinn HE, Pillsbury AJ, et al: Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child Adolesc Health. 2020. https://www.thelancet.com/action/showPdf?pii=S2352-4642%2820%2930251-0
10. Heavey L, Casey G, Kelly C, et al: No evidence of secondary transmission of nCOVID-19 from children attending school in Ireland, 2020. Eur Suerveill. 2020; 25: 2000903. DOI:10.2807/1560-7917.ES.2020.25.21.2000903
11. Yung CF, Kam KQ, Nadua KD, et al: Novel coronavirus 2019 transmission risk in educational settings. Clin Infect Dis. DOI:10.1093/cid/ciaa794
12. Danis K, Epaulard O, Benet T, et al: Cluster of coronavirus disease 2019 (Covid-19) in the French Alps, February 2020. Clin Infect Dis. 2020; 71: 825-32.https://www.thelancet.com/action/showPdf?pii=S2352-4642%2820%2930251-0
13. Link-Gelles R, DellaGrotta AL, Molina C, et al: Limited secondary transmission of SARS-CoV-2 in child care programs – Rhode Island, June 1 – July 31, 2020. MMWR 2020; 69: 1170-2.
14. Gilliam WS, Malik AA, Shafiq M, et al: COVID-19 transmission in US child care programs. Pediatrics. 2020. DOI: 10.1542/peds.2020-031971
15. 第12回新型コロナウイルス感染症対策アドバイザリーボード参考資料.https://www.mhlw.go.jp/content/10900000/000688926.pdf (2020年11月7日アクセス)
16. 文部科学省:学校における新型コロナウイルス感染症に関する衛生管理マニュアル〜「学校の新しい生活様式」〜(2020.9.3 Ver. 4) https://www.mext.go.jp/content/20200903-mxt_kouhou01-000004520_1.pdf (2020年10月11日アクセス)
17. Viner RM, Mytton OT, Bonell C, et al: Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults. A systematic review and meta-analysis. JAMA Pediatr. 2020. DOI:10.1001/jamapediatrics.2020.4573
18. Yung CF, Kam K, Chong CY, et al: Household transmission of severe acute respiratory coronavirus 2 from adults to children. J Pediatr. 2020; 225: 249-51.https://doi.org/10.1016/j.jpeds.2020.07.009
19. Bunyavanich S, Do A, Vicencio A: Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA. 2020; 323: 2427-9. DOI:10.1001/jama.2020.8707
20. Yonker LM, Neilan AM, Bartsch Y, et al: Pediatric severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Clinical presentation, infectivity, and immune responses. J Pediatr. 2020. DOI: https://doi.org/10.1016/j.jpeds.2020.08.037
21. Ludvigsson JF: Children are unlikely to be the main drivers of the COVID-19 pandemic – A systematic review. Acta Paediatr. 2020. DOI: https://doi.org/10.1111/apa.15371
22. Heald-Sargent T, Muller WJ, Zheng X, et al: Age-related differences in nasopharyngeal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) levels in patients with mild to moderate coronavirus disease 2019 (COVID-19). JAMA Pediatr. 2020; 174: 902-3. DOI: 10.1001/jamapediatrics.2020.3651
23. Kim J, Choe YJ, Lee J, et al: Role of children in household transmission of COVID-19. Arch Dis Child. 2020. DOI: 10.1136/archdischild-2020-319910
24. Castagnoli R, Votto M, Licari A, et al: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 2020; 174: 882-9. doi: 10.1001/jamapediatrics.2020.1467. https://jamanetwork.com/journals/jamapediatrics/fullarticle/2765169
25. 国立感染症研究所感染症疫学センター: NESIDに届出された20歳未満の新型コロナウイルス感染症例のまとめ (2020年2月1日〜5月28日). https://www.niid.go.jp/niid/ja/covid-19/9853-covid19-22.html
26. Zheng F, Liao C, Fan Q, et al: Clinical characteristics of children with coronavirus disease 2019 in Hubei, China. Current Medical Science 2020; 40: 1-6. https://link.springer.com/content/pdf/10.1007/s11596-020-2172-6.pdf
27. Bellino S, Punzo O, Rota MC, et al: COVID-19 disease severity risk factors for pediatric patients in Italy. Pediatrics. 2020; 146: e2020009399. DOI:https://doi.org/10.1542/peds.2020-009399
28. Cui X, Zhang T, Zheng J, et al: Children with coronavirus disease 2019 (COVID-19): A review of demographic, clinical, laboratory and imaging features in 2,597 pediatric patients. J Med Virol. 2020. https://doi.org/10.1002/jmv.26023
29. Gaborieau L, Delestrain C, Bensaid P, et al: Epidemiology and clinical presentations of children hospitalized with SARS-CoV-2 infection. J Clin Med. 2020; 9: e2227. DOI: 10.3390/jcm9072227
30. Mak PQ, Chung KS, Wong JS, et al: Anosmia and ageusia: Not an uncommon presentation of COVID-19 infection in children and adolescents. Pediatr Infect Dis J. 2020; 39: e199-200. DOI: 10.1097/inf.0000000000002718
31. Xia W, Shao J, Guo Y, et al: Clinical and CT features in pediatric patients with COVID-19 infection: different points from adults. Pediatr Pulmonol, 2020 Mar 05.https://onlinelibrary.wiley.com/doi/full/10.1002/ppul.24718
32. Whittaker E, Bamford A, Kenny J, et al: Clinical characteristics of 58 children with a pediatric inflammatory multisystemn syndrome temporally associated with SARS-CoV-2. JAMA 2020; 324: 259-69. DOI:10.1001/jama.2020.10369
33. Feldstein LR, Rose EB, Horwitz SM, et al: Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020; 383: 334-46.DOI:10.1056/NEJMoa2021680
34. Dufort EM, Koumans EH, Chow EJ, et al: Multisystem inflammatory syndrome in children in New York state. N Engl J Med. 2020; 383: 347-58.DOI:10.1056/NEJMoa2021756
35. Davies P, Evans C, Kanthimathinathan HK, et al: Intensive care admission of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: a multicenter observational study. Lancet Child Adolesc Health. 2020; 4: 669-77.DOI:10.1016/S2352-4642(20)30215-7
36. 日本川崎病学会:川崎病とCOVID-19に関する報道について【参考資料】www.jskd.jp/pdf/20200508COVID-19andKD.pdf (2020年10月13日アクセス)
37. Uda K, Okita K, Soneda K, et al: Kawasaki disease following coronavirus disease 2019 with prolonged fecal viral shedding. Pediatr Int. (accepted)
38. Xu CLH, Manjri R, Schnall JA, et al: Duration of respiratory and gastrointestinal virus shedding in children with SARS-CoV-2: a systematic review and synthesis of data. Pediatr Infect Dis J. 2020.DOI:10.1097/INF.0000000000002814
39. Bahar B, Jacquot C, Mo YD, et al: Kinetics of viral clearance and antibody production across age groups in children with severe acute respiratory syndrome coronavirus 2 infection. J Pediatr. 2020.https://doi.org/10.1016/j.jpeds.2020.08.078
40. 日本小児科学会予防接種・感染症対策委員会:小児におけるCOVID-19治療薬に対する考え方(第1版)http://www.jpeds.or.jp/modules/activity/index.php?content_id=346
41. Elshafeey F, Magdi R, Hindi N, et al: A systematic scoping review of COVID-19 during pregnancy and childbirth. Int J Gynaecol Obstet. 2020; 150: 47-52. doi: 10.1002/ijgo.13182. https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1002/ijgo.13182
42. Allotey J, Stallings E, Bonet M, et al: Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ 2020; 370: m3320.http://dx.doi.org/10.1136/bmj.m3320
43. Goh XL, Low YF, Ng CH, et al: Incidence of SARS-CoV-2 vertical transmission: a meta-analysis. Arch Dis Child Fetal Neonatal Ed. DOI:10.1136/fetalneonatal-2020-319791
44. Chambers C, Krogstad P, Bertrand K, et al: Evaluation for SARS-CoV-2 in breast milk from 18 infected mothers. JAMA 2020; 324: 1347-8. DOI:10.1001/jama.2020.15580
45. Dumitriu D, Emeruwa UN, Hanft E, et al: Outcomes of neonates born to mothers with severe acute respiratory syndrome coronavirus 2 infection at a large medical center in New York City. JAMA Pediatr. 2020. DOI:10.1001/jamapediatrics.2020.4298
46. Han MS, Seong MW, Heo EY, et al: Sequential analysis of viral load in a neonate and her mother infected with SARS-CoV-2. Clin Infect Dis. 2020 Apr 16. pii: ciaa447. doi: 10.1093/cid/ciaa447. https://academic.oup.com/cid/article/doi/10.1093/cid/ciaa447/5820869
47. Kanburoglu MK, Tayman C, Oncel MY, et al: A multicentered study on epidemiologic and clinical characteristcs of 37 neonates with community-acquired COVID-19. Pediatr Infect Dis J. 2020; 39: e297-302.
48. Wang X, Pasco RF, Du Z, et al: Impact of social distancing measures on coronavirus disease healthcare demand, Central Texas, USA. Emerg Infect Dis. 2020; 26: 2361-9. https://dx.doi.org/10.3201/eid2610.201702
49. Bayham J, Fenichel EP: Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. Lancet Public Health. 2020 Apr 3; 5: E271-8. pii: S2468-2667(20)30082-7. doi: 10.1016/S2468-2667(20)30082-7. https://www.thelancet.com/pdfs/journals/lanpub/PIIS2468-2667(20)30082-7.pdf
50. Davies NG, Klepac P, Liu Y, et al: Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020; 26: 1205-11.https://www.nature.com/articles/s41591-020-0962-9
51. Viner RM, Russell SJ, Croker H, et al: School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020 Apr 6. doi: 10.1016/S2352-4642(20)30095-X https://www.thelancet.com/pdfs/journals/lanchi/PIIS2352-4642(20)30095-X.pdf
52. Rice K, Wynne B, Martin V, et al: Effect of school closures on mortality from coronavirus disease 2019: old and new predictions. BMJ. 2020; 371: m3588. http://dx.doi.org/10.1136/bmj.m3588
53. Islam N, Sharp SJ, Chowell G, et al: Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. 2020; 370: m2743. DOI: 10.1136/bmj.m2743
54. Yehya N, Venkataramani A, Harhay MO: Statewide interventions and Covid-19 mortality in the United States: an observational study. Clin Infect Dis. 2020. ciaa923. DOI: 10.1093/cid/ciaa923
55. Xie X, Xue Q, Xie X, et al: Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020; 174: 898-900. doi: 10.1001/jamapediatrics.2020.1619.https://pubmed.ncbi.nlm.nih.gov/32329784/
56. Courtney D, Watson P, Battaglia M, et al: COVID-19 impacts on child and youth anxiety and depression: challenges and opportunities. Can J Psychiatr. 2020; 65: 688-91. https://doi.org/10.1177/0706743720935646
57. Goldman PS, van Ijzendoorn MH, Sonuga-Barke EJS, et al: The implications of COVID-19 for the care of children living in residential institutions. Lancet Child Adolesc Health. 2020; 4: e12. doi: 10.1016/S2352-4642(20)30130-9.
58. Lawson M, Piel MH, Simon M: Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. 2020. DOI: 10.10106/j.chiabu.2020.104709.
59. Greeley CS: Child maltreatment prevention in the era of coronavirus disease 2019. JAMA Pediatr. 2020. DOI:10.1001/jamapediatrics.2020.2776
60. NPO法人 全国こども食堂支援センター むずびえ. こども食堂の現状&困りごとアンケート Vol. 3. https://musubie.org/news/2601/ (2020年11月7日アクセス)
61. UNICEF warns COVID-19 may reverse child health progress. https://www.aa.com.tr/en/latest-on-coronavirus-outbreak/unicef-warns-covid-19-may-reverse-child-health-progress/1968122 (2020年11月7日アクセス)
62. World Health Organization: WHO and UNICEF warn of a decline in vaccinations during COVID-19. https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19 (2020年10月13日アクセス)
63. 日本小児科学会 予防接種・感染症対策委員会:新型コロナウイルス感染症流行児における小児への予防接種について. http://www.jpeds.or.jp/uploads/files/20200617_yobosesshu.pdf (2020年10月13日アクセス)
64. 古賀大貴、本村良知、松岡若利、他:コロナウイルス感染症2019拡大に伴う医療機関受診抑制による重症百日咳乳児例. 日本小児科学会雑誌(2020年10月12日採択)
会員・医療関係者 各位
2020年 5 月20日 第1報
日本小児科学会予防接種・感染症対策委員会
「小児の新型コロナウイルス感染症に関する医学的知見の現状」を作成いたしましたので、ご確認ください。
小児の新型コロナウイルス感染症に関する医学的知見の現状